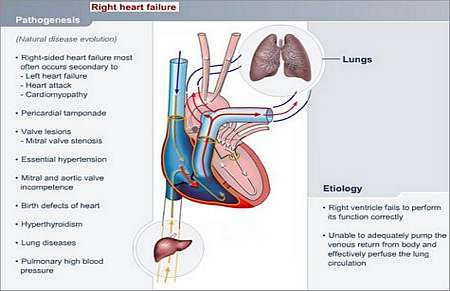
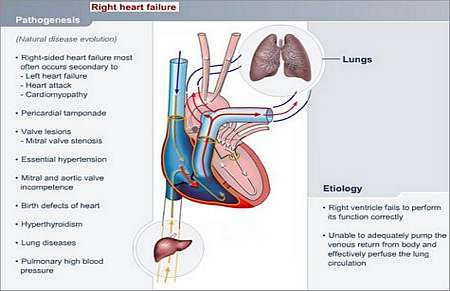
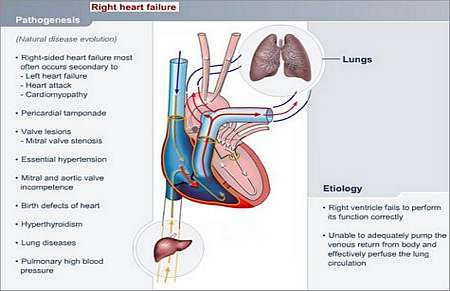
What is RIGHT HEART FAILURE?
The right heart fails to function correctly. The right side of the heart (right lower heart chamber) is unable to effectively pump blood, which returns to it via large veins (superior and inferior vena cava) from the rest of the body, through the lung circulation to the left heart chambers.
Why does this happen and how may it affect the patients health?
Right heart failure mostly occurs as a consequence of left heart failure.
The left heart may be failing because of
- A heart attack in the left heart muscle
- Valve lesions on the left heart side
- High blood pressure
- Fluid in the pericardial sac (pericardial tamponade)
Other causes of right heart failure
- An overactive thyroid gland
- Birth defects of the right or left heart
- Diseases of the lungs, such as increased pressure inside blood vessels of lung circulation due to narrowing (pulmonary hypertension), or lung tissue diseases that cause pulmonary hypertension (Cor pulmonale) leading to right heart failure
- Emphysema
- Blood clots in the lung (pulmonary embolism secondary to trombo-embolic disease)
What symptoms may the patient experience?
- Shortness of breath
- Fast heart rate (more than 120 beats per minute)
- Orthopnoea (shortness of breath when lying down)
- Feeling tired
- Feeling weak
- Pain and swelling of the abdomen, which may be caused by an enlarged liver (the liver may feel firm and tender), congested veins inside the liver, or ascites (accumulation of fluid in the abdomen).
- The patient may experience mental changes due to reduced oxygen and blood pumped to the brain (more commonly seen in severe forms of heart failure; especially in the elderly)
- Neck veins may become visibly distended
- Fluid may accumulate between the lungs and the chest wall (pleural effusion)
- Changes on the skin surface may include Spider naevi, liver palms (reddish palms) and painful breast and nipple tissue
- Jaundice (yellow discoloration of skin and eyes secondary to excessively high bilirubin concentration in blood; bilirubin is a breakdown product of blood) in late stages
- Extremities (feel cold; appear pale)
- Patient loses weight
- There may be swelling of the ankles
How is the diagnosis made and what special investigations are required?
- ECG: Assessment of electrical activity of the heart. May show right ventricular strain pattern.
- X-ray of the chest: May show congested veins in lungs.
- X-ray of the abdomen: May show an enlarged liver, or fluid in the abdomen (ascites).
- Sonar of the heart: To assess heart size and lesions.
- Heart catheterisation: May be done to examine coronary blood-flow, and rule out valve and wall lesions.
What is the treatment and prognosis?
- Oxygen
- Bed rest in fowler position (incline upper body at 30 to 40 degree angle)
- Elevate legs
- Remove precipitating causes
- Treat the heart failure itself
- Restriction of physical activity
- Restriction of salt intake via diet or otherwise
- Medication includes Diuretics, Digoxin, Vasodilators or Inotropes (drugs that enhance heart muscle contraction).
- Hospitalisation may be necessary
- A heart transplant may be considered in terminal cases
Prognosis depends on
- The underlying cause of heart failure
- Whether the underlying cause can be treated effectively
- The severity of heart failure
- The damage caused by heart failure
- Duration of heart failure
- The patients age
- The patients compliance with treatment protocols
© 2003 Prometheus™ Healthcare (Pty) Ltd
|